Authored by Dr. Susan E. Brown, PhD
It was once believed that age was the determining bone health risk factor for women. If you were over 50, then you were automatically considered at high risk for bone problems. We know so much more about bone loss, osteoporosis and bone health risk factors than just a few decades ago – great news for any woman determined to have stronger bones for life.
Is age a factor in the health of your bones? Yes. However, it’s just one factor, and usually not the deciding one. We now have a much better understanding of the many factors that affect your bone health and influence your chances for excessive bone loss, osteoporosis or experiencing a fracture. And here’s the great news — many of these factors are ones that you have the ability to change in your favor.
Table of contents
Look through the list of bone health risk factors and read about what could be impacting your bones. No matter how many factors you may have, feel confident. You can reduce your risk and strengthen your bone health!
Hormonal imbalance
Prior to menopause, ovulation is orchestrated by the production of estrogen and progesterone, among other hormones. Estrogen and progesterone have positive effects on bone health. They increase the absorption of calcium and lessen the loss of calcium from bones. Estrogen also has an inhibiting effect on parathyroid hormone, which is a bone-breakdown hormone.
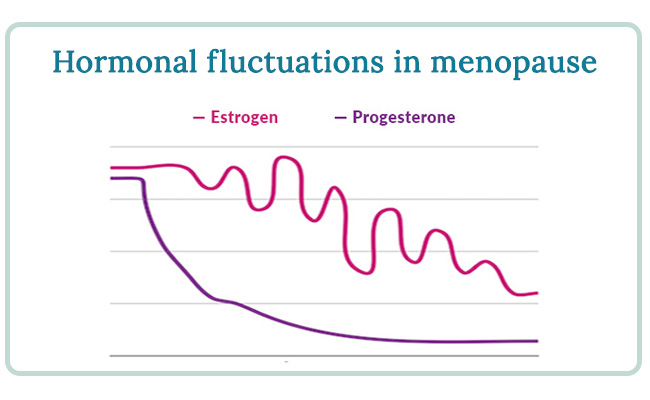
You may have heard that women can lose as much as 20% of their bone mass as they transition through menopause. I want to clear up that what’s creating this risk for excess bone loss is not menopause itself. Rather, it’s the hormonal imbalances that commonly develop during perimenopause and menopause that appear to be the main culprit. You can get through menopause without a hormonal imbalance, and that’s key.
During menopause, sex hormone levels fluctuate and decline. Menopause is a natural transition, not a disease, and in otherwise healthy and balanced women, bone has a sufficient surplus of mass to remain strong indefinitely after menopause. However, many women go through perimenopause and menopause in a state of hormonal imbalance, and this may be part of what puts some women’s bones at risk for excessive loss.
For example, noted Canadian endocrinologist Dr. Jerilynn Prior and others have conducted research on the effects of progesterone on bone loss during menopause. Progesterone, in many cases, is the hormone to decrease first in perimenopause; as it does, it often falls into an imbalanced ratio with estrogen. Dr. Prior’s work shows that progesterone and our bone-building cells, called osteoblasts, have a complex relationship and progesterone may help build bone. When there is a hormonal imbalance, progesterone levels are effectively “squashed” and may not be sufficient to carry on this work.
If you’re menopausal, paying close attention to hormonal balance is one key to building stronger bones for life. You can’t reverse menopause, nor do you need to, but you have many options for building and maintaining natural bone health during menopause and beyond.
Low bone density
Nearly every woman I talk to thinks that low bone density is the greatest threat to her bone health. She believes that thin bones are prone to fracture, and that dense bones are strong enough not to break. The truth is — yes, some women with low bone density will suffer a fracture, but so will some women with denser bone. Bone density alone does not seem to be a single determining risk factor.
The research on this point is clear: in one study of hip fractures in women, only 57% of women who fractured had low bone density, while 27% had medium bone density and 16% had high bone density! Keep in mind, 95% of the women in this study did not fracture at all, regardless of their bone density.
In fact, research shows that a severely osteoporotic vertebra with only 50% of its normal amount of bone is still strong enough to withstand five times its normal strain load. This helps explain why in some countries, like France, Germany, China and Japan, women on average have lower bone density than in America, yet experience far fewer osteoporotic fractures. Low bone density is simply not the real problem.
Have you had your bone density tested?
There is no direct measure of bone quality or strength, but there is a test for bone density, which is how some of the confusion arises. Conventional medicine likes to treat problems it can measure — and bone density is no exception. Unfortunately, treating bone density exclusively doesn’t always result in healthier bones. Dense bones that are composed of old, stagnant tissue can be brittle and prone to fractures.
This is one of the major risks of bone density drugs (bisphosphonates) like Fosamax and Boniva. Bone density drugs stop the breakdown of bone, allowing minerals to accumulate and resulting in greater bone density, but without breakdown there is no repair. Within a year of using bone density drugs, the action of bone-building cells stops entirely. The resulting bone is dense, but usually poor quality and sometimes quite fragile.
So what does low bone density really say about your bone health?
Low bone density alone may not cause fractures, but this is not to say that bone loss doesn’t matter. Excessive bone density loss is an indication that your bone metabolism is out of balance, which means your bones are struggling to keep up with demands.
Bone loss is not an isolated condition, nor does it mean your bone metabolism is faulty. Bone loss is usually a result of systemic imbalances elsewhere in the body. For example, if your body has a high acid burden, your bones donate their minerals to maintain the necessary blood pH level. If your body is receiving inadequate nutrition, your bones allow other organs to take their share first. These sacrifices are necessary for survival, but can cause bone breakdown to happen at a faster pace than new bone is formed, which may result in lower bone density and poor quality bone.
Build better bones, not just denser bones
Rather than simply treating symptoms — like low bone density — we should ask ourselves, How can we heal the underlying bone metabolism imbalance? That is, how can we reduce the factors that accelerate bone loss and increase the activity of cells that build new bone? How can we do this without drugs?
When we take this approach we see improvements in bone quality and strength, rather than bone density alone. It works by supporting your bones’ natural self-repair mechanisms, reducing the burden on your bones and encouraging healthy new bone formation. Many women find their bone density increases with this natural approach to bone health, but more important the quality of the bone improves. The basic approach we recommend is:
- An alkaline diet to help your bones conserve minerals.
- Nutritional support to your bone-building cells.
- Lifestyle changes, including exercise and stress relief.
Bone density is a risk factor you have some control over — but it isn’t the definitive measure of bone health that most women think it is. Understand that the real opportunity for preventing fractures is building strength, not density alone. The good news is there’s a lot you can do to strengthen your bones, without drugs.
pH imbalance
Most new patients who come to our healthcare clinic aren’t familiar with pH balance. And yet restoring an alkaline pH level is one of the most powerful things you can do for your bone health.
pH refers to a measurement of the acidity or alkalinity of a substance. Low pH readings (below 7.0) are considered acidic, while higher readings (above 7.0) are considered alkaline. Your body functions best when its blood pH is slightly alkaline (between 7.35 and 7.45), but many of its processes — like digestion of certain foods — produce acid residues. This means your pH level is always in flux: acids are constantly being produced and neutralized.
Your bones are the guardians of pH. While your body has several mechanisms for dealing with internal acid production — such as excreting it through the lungs and kidneys — your bones are a vital safety net for your pH. Bones store alkalizing mineral compounds, which they donate as needed to neutralize acids.
Bone — the great giver
It may seem hard to believe, but even tiny fluctuations in the blood pH can have profound effects on your health. A shift of just 0.1 from the ideal range causes blood cells to be unable to deliver adequate oxygen and protect us from disease. Other body tissues have a much wider range of acceptable pH levels, but blood pH must be tightly regulated.
If it weren’t for the mineral reserves in your bones, you would have to consume a precise amount of minerals on a daily — or even hourly — basis to prevent acidosis in the blood. Fortunately, bones store these minerals for us and readily donate them when needed.
This process is literally life-saving, so it’s no wonder that bones have evolved to prioritize pH balance over their other responsibilities, like building strength and resisting fracture. With a healthy balance between acid production and nutrient intake, your bones can easily do both. However, when acid production chronically outpaces nutrient intake, bone strength deteriorates.
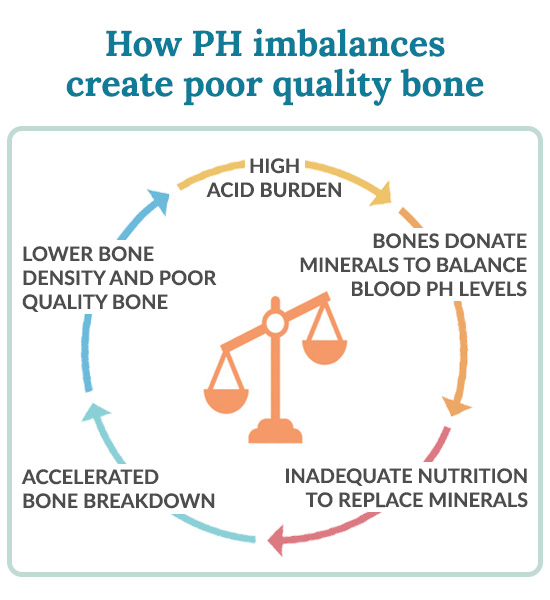
Balance your diet to balance your pH
Unfortunately, most Americans today eat too many acid-forming foods — so many that our bones are often unable to keep up with neutralizing them. Acid is produced during the digestion of animal protein, sugar, processed foods, salt and coffee — substances that permeate the average American diet. Chronic inflammation, exposure to toxins and stress also have an acidifying effect on the body.
The good news is you can improve your pH by following an alkaline diet. When you do, your bones will divert fewer resources towards neutralizing acids and be better able to repair and strengthen.
Inactivity
Physical activity is the foremost stimulator of bone. When you exercise, your muscles exert tension and compression on your bones, which respond by stimulating bone formation.
If you’re looking for a simple way to reduce your risk of fracture dramatically, start an exercise program. Research shows that women who engage in regular exercise have one-half to one-third the fracture risk as women who do not exercise!
Bone responds to the demands placed on it. When you engage in exercise — especially weight-bearing exercise — you are literally telling your bones to become more resilient. On the other hand, bone seeks to be no heavier than necessary and will become lighter and thinner if we are physically inactive.
Exercise also benefits you by helping maintain mobility and balance as you age. Falls are the leading cause of fracture in the elderly, and when you are physically fit and strong you are less likely to fall.
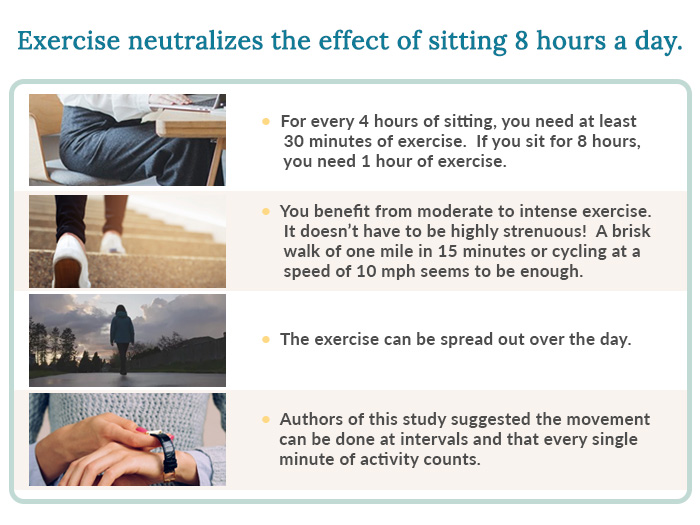
Research suggests that women doing vigorous exercise twice a week or total physical activity of four hours a week have significantly higher bone density than women with lower activity levels. Vigorous exercise is generally needed to build bone, but even less strenuous forms of exercise like moderate walking can help prevent further bone loss. In short, any amount of physical activity is beneficial to your bones.
Insufficient nutrition
Nutrition provides the building blocks of all the cells in our body. Our health, on every level, depends upon vitamins and minerals to function — and to function well.
When it comes to bone health, your diet is one of the simplest, most powerful tools you have for protecting and strengthening your bones. And yet many women who follow a “healthy” diet get osteoporosis anyway. So what kind of potential does your diet have for protecting your bones, and how do you make the most of it?
Your diet may not be as nutritious as you think
Your skeleton is the most altruistic of your organs (yes, the skeleton is an organ, just like your heart, skin or spleen). When nutrition is in short supply, the bones allow other organs to meet their needs first. Like many women, their own needs come after the needs of those around them.
And even when we try to make healthy food choices we are at a disadvantage. Modern food production has depleted our soils of minerals, causing food grown in those soils to have fewer nutrients. Vegetables and fruit are usually harvested when unripe and allowed to ripen while being shipped over long distances, meaning those foods have less time to draw nutrients from the sun and soil as they are growing. As a result, insufficient nutrition is the norm, and our bone health suffers.
What about calcium?
Ironically, one nutrient that Americans get more of than most other countries is calcium, and yet bone fractures are more common in American women than women in other cultures.
Our over-reliance on calcium to support bone health disguises the fact that bones require a range of nutrients — at least 20 that research has identified — for optimal health. Some of these nutrients, like vitamins D and K, work by helping the body use calcium, and others work independently of calcium.
Nutritional supplements help fill the gaps
Consuming nutritious foods will go a long way toward providing your bones with the nutrients they need, but even the best diet usually falls short of the level of nutrition needed for optimal bone health. A high-quality nutritional supplement for bone can help fill those gaps.
Dietary excesses
Certain substances directly interfere with bone building or otherwise damage bone health. Reducing or eliminating those substances from your diet can go a long way in protecting your bone health.
- Sugar increases the excretion of valuable nutrients, including calcium, magnesium, chromium, copper, zinc and sodium. It also limits calcium absorption, and is highly acid-forming, causing still more mineral loss from bone.
- Soda, especially cola, contains phosphoric acid, which leaches calcium from bone. It also prevents absorption of magnesium, a key bone-building mineral. Soda’s high sugar content acidifies the body.
- Sodium, in the form of sodium chloride or table salt, is second only to sugar as the most popular food additive. Salt increases secretion of calcium in the urine. Increasing your calcium intake can help compensate for excess sodium, but any woman consuming more than 2000 mg of sodium per day (the average American consumes 8000 mg per day) can reduce bone breakdown simply by decreasing her salt intake.
- Protein is necessary for the formation of collagen in bone, but too much dietary protein erodes your bones. Digestion of protein (particularly animal protein) creates acids that must be neutralized with the alkalizing mineral compounds stored in your bones. Most Americans eat far more animal protein than is necessary, and the excess drains your bone of the minerals it needs to remain healthy and strong.
- Alcohol negatively affects bone health on many levels. It inhibits absorption and increases secretion of calcium, magnesium, Vitamin C, zinc and copper. It damages the liver, which can interfere with Vitamin D metabolism, and directly decreases the spongy inner trabecular bone.
The good news is that avoiding these substances is a simple way to improve your bone health by immediately reducing the demands on your bones. And you don’t have to totally eliminate them to get some of the benefits. Even reducing your consumption will help limit the negative effects on your bones. The more you avoid dietary excesses, the better for your bones.
Indoor lifestyle
Most of us live, work and play indoors. Why does this matter for our bone health? When your skin is exposed to the ultraviolet B rays in sunlight, it produces Vitamin D, one of the most vital nutrients for bone health. Vitamin D is crucial for calcium absorption, among other things.
Despite the seemingly abundant availability of Vitamin D — it’s as accessible as sunlight — many women have insufficient levels of the nutrient. With busy lives and inclination towards indoor activities, most women simply don’t get outside to soak up enough sun. When we are outdoors, we often use sunblock to protect against the sun’s harmful effects, and unfortunately this also blocks its ability to stimulate Vitamin D production. Women living in North America and northern parts of Europe and Asia are particularly prone to Vitamin D deficiency because between the months of October and April, too little UVB penetrates the atmosphere in the northern latitudes to synthesize Vitamin D. (Not to mention the fact that cold weather makes us limit our skin exposure to the sun!)
The good news is that Vitamin D deficiency is easy to fix. As little as 20 minutes of sunlight per day on your face and arms (without sunscreen) is enough for women with light skin to maximize their Vitamin D. If you have dark skin you may need as much as 90 minutes or more. Taking a brisk walk outdoors is a great way to combine Vitamin D production with the bone-building effects of exercise.
If you can’t get outside, if you live in a northern latitude or if the weather doesn’t allow for sun exposure, you can easily get your Vitamin D other ways. Foods high in D include mackerel, sardines, egg yolks and fortified milk. You can also get Vitamin D through the efficient option of nutritional supplementation.
Digestive issues
You may eat a healthy diet. You may take all the right nutritional supplements. But if you can’t digest all those nutrients and transport them to your cells, they’re not doing you much good. Robust digestion is crucial to bone health.
We tend to think that unless we have a bowel-related disease, a few digestive symptoms are “normal.” But even mild digestive issues can harm our nutrient absorption, and when these problems are chronic, real nutritional deficiencies can develop. Of the 20 bone-building nutrients you need every day, calcium is particularly vulnerable to poor absorption.
Digestive problems can have many causes, but the most common causes are:
- Unidentified food allergies or sensitivities. Many women have a low-grade allergy or sensitivity to certain foods. Because the allergic response in these cases is more mild or delayed compared to an acute allergic reaction, they can go unidentified for years. You may have occasional gas, bloating, diarrhea, intestinal cramping, headaches or irritability without connecting your symptoms to a specific food or ingredient. Some of the most common culprits are sugar, wheat (gluten), coffee, eggs, milk, corn, nuts and shellfish.
- Intestinal flora imbalance. Healthy digestion depends on millions of microbes that reside in your intestines. These tiny bacteria help break down nutrients for digestion, as well as manufacture certain vitamins, support your immune system and metabolize hormones. But these “friendly flora” are in competition with harmful bacteria that also seek to colonize your GI tract. If your diet is low in fiber and high in sugar and fat, or if you frequently take antibiotics, harmful bacteria can get the upper hand while the good guys die off by the millions.
If you have frequent or occasional digestive symptoms, it’s time to figure out why. Not only can you solve your symptoms, but you’ll also ensure that the nutrients you eat are reaching your cells, including those in your bones.
Fortunately, there’s a lot you can do to heal your GI tract. We’ve had great success helping women heal their digestion and get the most from their nutrition.
Family history
If your biological mother or father has fractured a hip, you have a statistically higher risk of experiencing a fracture yourself.
Obviously there’s nothing you can do about your family history of fracture. But consider it encouragement to prioritize your bone health, and learn from your family member’s experience.
Every individual has a unique bone burden, and the factors that caused your parent’s fracture may not apply to you, or may not cause you to fracture also. Take heart in knowing that your genetic makeup is not your destiny, and there are plenty of opportunities for you to start taking control of your bone health.
Previous fracture
If you’ve fractured a bone as an adult you know what a threat fractures can be to your health and quality of life. But we want to assure you that it’s not too late to strengthen your bones and prevent future fractures.
Oftentimes women who have had a fracture are so shaken by their experience that they begin treating their bodies as though they were fragile and delicate, restricting their activities and avoiding placing too much strain on their bodies. This is unfortunate because exercise is just what you need to prevent another fracture! But before you can get back on your feet you have to regain some confidence in your bones.
The fact that you’ve had a fracture is not a bone health risk factor you can change, but you can take action every day to make sure it doesn’t happen again. The basic approach we recommend is:
- An alkaline diet to reduce the demands on your bones
- Medical-grade nutritional supplements to give your bone-building cells the support they need, especially including Vitamin D
- Regular exercise
- Stress relief
- Avoiding substances that weaken bone
Be mindful of the fact that certain exercises like high-impact activities may not be appropriate for women who have already had a fracture caused by bone fragility. But there are still plenty of options for you to exercise to better bones.
No matter what the current state of your bone health, it’s never too late to get started.
Low body weight
We hear a lot in the media about the health risks of being overweight. But being underweight comes with its own set of risks — one of which is an increased risk of osteoporosis and fracture.
In fact, weighing less than 120 pounds is one of the strongest risk factors for poor bone health. There are a few reasons why. Having lower body weight means you tend to have less muscle mass, and bone mass is closely related to muscle mass. Thin women also generally eat less, and may be less likely to consume sufficient nutrition for bone building. Finally, if a woman’s body fat is too low, her periods will become irregular or will stop altogether, which is a major risk factor for poor bone health.
If you’re underweight, you owe it to your bones to gain a few pounds. But don’t take this as a green light to eat processed and sugary foods. Healthy weight gain means eating larger portions of healthy foods, or eating more often during the day. You may also have to reduce your level of physical activity if you exercise a lot. All that activity won’t help your skeleton unless it has the nutrition it needs to build bone.
Gaining weight is as difficult for some women as losing weight is for others. Our patients have had the most success when they focus on maximizing nutrient intake. The nutritional guidelines in our Better Bones protocol will help you choose the right foods for healthy weight gain.
Emotions and stress
Stress and emotions are both powerful bone health risk factors.
Your body responds to stress by producing a hormone called cortisol. Cortisol has many effects on the body, one of which is mobilizing calcium from bone and increasing its secretion through the urine. In other words, when you’re stressed, your bones begin spilling the minerals they need for bone formation into the bloodstream for the good of other tissues. Unfortunately, most of us experience chronic stress, which means your bones are continuously leached of minerals, which often aren’t being replaced in the diet.
Depression also negatively impacts bone health. Research shows women with past or present depression have lower bone density than women who have never experienced depression. One explanation for this link is that depression increases cortisol production, much like stress does. Depressed women are also less likely to consume sufficient nutrition for bone health, and are less likely to be active.
Clearly, our emotions play an important role in our bone health. And most women have certain sources of stress that they can’t avoid. But we do have the ability to change the way we respond to stress, and lessen its impact on our health.
Exercise can be a wonderful stress reliever, with the added benefit of directly stimulating bone formation. We also recommend meditation, deep breathing and sleeping at least 7-8 hours per night. Simple dietary changes and medical-grade nutritional supplements can help heal the damaging effects of stress on our adrenals, the glands responsible for producing cortisol.
Toxins
Exposure to certain toxins can damage your bone health. Our modern environment exposes us to a range of pollutants, chemicals and heavy metals every day. Although your body is equipped with mechanisms for removing toxins, the unprecedented number of substances in our environment can be overwhelming.
When it comes to bone health risk factors, heavy metal exposure is particularly harmful. Metals are not easily excreted by the lymphatic system, and tend to accumulate in the body.
- Lead inhibits activation of Vitamin D and limits calcium absorption. It can be stored in the bones, displacing calcium, and released as bones begin to break down after menopause. This may exacerbate menopausal bone loss. There is some evidence that lead also interferes with progesterone levels, preventing that hormone’s beneficial effects on bone health.
- Cadmium damages the kidneys and alters calcium metabolism.
- Aluminum lessens calcium absorption, interferes with bone mineralization and modifies collagen production within the bones.
Other substances that are toxic to bone include mercury, tin and pesticides.
It should come as no surprise that we recommend avoiding heavy metals and toxins as much as possible. Unfortunately, our environment is inundated with them, and it isn’t possible to eliminate our exposure entirely. We recommend supporting the bioregulatory processes that clear toxins from your body, drinking plenty of filtered water, exercising daily and incorporating our bestselling liver support formula to nourish your most important detox organ.
Smoking
If you smoke, you probably already know you should quit to reduce your risk of cancer and heart disease. But you may not be aware of the effects smoking has on your bones.
- Smoking significantly increases the chance that you will experience an osteoporotic fracture.
- Smoking leads to poor Vitamin D status, which in turn can affect calcium absorption and metabolism.
- The anti-estrogenic effect of smoking exacerbates the negative effects of hormonal imbalance on your bones.
- Smoking depletes the body of vital bone-building nutrients, especially Vitamin C.
- Smoking increases the body’s toxic burden of cadmium, lead, nicotine and dozens of other toxic substances that interfere with calcium absorption and damage bone.
- Smokers who fracture a bone heal more slowly than non-smokers. Smokers are also less able to heal the microfractures that occur on a regular basis in our bones, leading to poor bone quality.
In short, the more you smoke the more damage you do to your bones. Quitting smoking is a great opportunity to quickly improve your bone health. The good news is that once you stop smoking, you can reverse the negative effects smoking has had on your bones.
Inflammation
Many women suffer unknowingly from chronic inflammation. Inflammation accelerates bone breakdown by triggering activity in the cells that demineralizes bone, called osteoclasts.
We’re not talking here about acute inflammation, which is the response to an injury or infection and is a lifesaving process. Although acute inflammation also triggers bone breakdown, the benefits of the simultaneous immune response outweigh any short-term effects on your bones. The problem arises when low-grade inflammation lingers in the absence of an injury or infection. When this occurs, the immune system is on constant alert and your osteoclasts remain overstimulated, breaking down bone at a faster rate than new bone is built.
If you suffer from joint pain, allergies, acne, psoriasis, eczema, asthma or digestive problems, there’s a good chance that chronic inflammation is affecting you. Getting your inflammation under control will help restore balance to your bone metabolism, and reduce your risk of weak bones.
Fortunately, there’s a lot you can do to heal chronic inflammation. We recommend:
- An annual detoxification diet to help clear your body of toxins that trigger the inflammatory response
- Regular exercise
- Avoiding processed foods, sugar, refined carbohydrates and any food to which you have a sensitivity
- Supplement with essential fatty acids — specifically, Omega-3 fatty acids are natural anti-inflammatories, which is why we include them in our Better Bones Combos.
Reducing inflammation has widespread benefits for your body, and is especially important if you’re interested in healing your bones and preventing fracture.
Medications
Often overlooked among bone health risk factors is the variety of prescription medications which directly cause excessive bone loss. These include: corticosteroids, synthetic thyroid hormones, aluminum-containing antacids, some diuretics, anticonvulsants and antibiotics.
Other medications, like tranquilizers, sedatives and antidepressants, increase your risk of fracture by increasing the chance of falling.
Different drugs affect bone health in different ways. Some diuretics increase calcium secretion, while long-term use of anticonvulsants is associated with Vitamin D deficiency. Aluminum (contained in many antacids) inhibits calcium absorption and interferes with mineralization and collagen synthesis. Aluminum is particularly harmful in people with low calcium intake.
Corticosteroids like cortisone and prednisone are given to treat inflammatory conditions, including allergies, lupus and arthritis. They harm bone health on several levels: they interfere with collagen synthesis, increase parathyroid hormone, inhibit calcium absorption, increase calcium secretion, impair bone formation and accelerate bone breakdown.
Although antibiotics don’t seem to affect bone metabolism directly, they have the effect of killing off important microorganisms in the intestines that are vital for optimal nutrient absorption. Overuse of antibiotics may lessen the availability of nutrients to your bone-building cells. We recommend you pair any antibiotic use with a course of probiotics, if you don’t take them already.
Depending on your individual circumstances you may not be able to avoid a certain medication. We recommend using the lowest effective dose for the shortest amount of time necessary. When possible, look for natural alternatives. For example, most women can avoid antacids with dietary and lifestyle changes that promote healthy digestion.
When you can’t avoid a medication that’s harmful to your bones, it’s all the more important to support your bone health in other ways. We’ve had great success helping women mitigate the harmful effects of necessary drugs by reducing other demands on bone and providing holistic support to bone-building cells.
Diseases
In conventional Western medicine, there is a technical distinction between “primary” and “secondary” osteoporosis. Primary osteoporosis is what most of us think of when we talk about bone health — its causes are complex and it occurs as a discrete diagnosis. Secondary osteoporosis is caused directly by another disease or condition, and it is diagnosed in conjunction with that condition. Secondary osteoporosis should always be ruled out when excessive bone loss occurs.
Causes of secondary osteoporosis include:
- Hyperparathyroidism
- Cushing’s Syndrome
- Hypogonadism
- Hyperthyroidism
- Diabetes mellitus
- Lymphomas
- Sickle cell disease
- Osteogenesis imperfecta
- Scurvy
- Chronic renal failure
- Malabsorption
- Myeloma
Bone health risk factors: your risk is not your destiny
When women are concerned about their bone health risk factors, I always remind them that their own blend of bone health risk factors did not develop overnight. In fact, you’ve been living with them for quite some time and haven’t fractured yet. So take heart. Being at risk for a certain event does not cause it to occur. It simply means you should be aware of your body’s unique needs.
If you have already been diagnosed with osteoporosis or experienced a fracture, don’t be dismayed. It’s never too late to improve the health of your bones. You may have to work a little harder at it because of your starting point, but we promise you it’s possible to build bone regardless of your current bone health status.
This may be a message you haven’t heard before. But we have helped thousands of women dial down their risk of fracture and other bone health risk factors, and we can help you too. So let’s start by understanding the state of your bone health. Take our free Bone Health Quiz to get your list of personalized bone health risk factors.













