Authored by Dr. Mary James, ND
Our surveys of over 7 million women have revealed the most commonly experienced symptoms of hormonal imbalance. Let’s talk about these main symptoms and where they come from — then we’ll discuss what you can do to find relief.
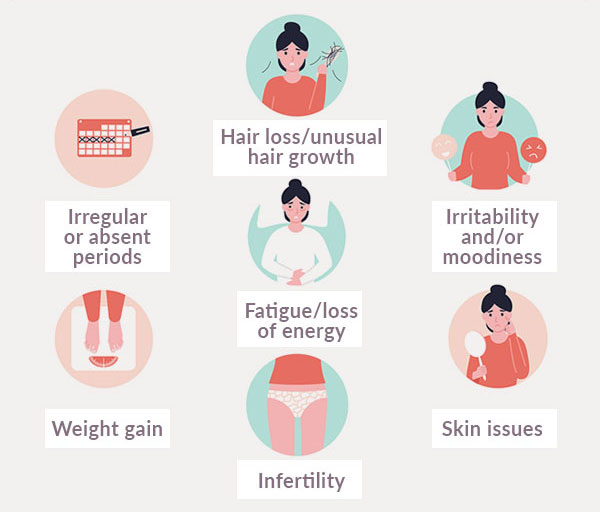
- Irregular or absent periods: Increasing irregularities in your period signal a disruption in the hormonal activity that controls menstruation. Often, the cause is an imbalance between estrogen and progesterone due to the strong effects of the stress hormone, cortisol.
- Weight gain: Changes to your weight or body shape, particularly in menopause, are caused by shifting hormones that tell your body to store fat in the abdomen. This can occur even if you’ve never had a weight problem before. High stress and poor sleep increase belly fat, which can then be difficult to lose.
- Irritability and/or moodiness: Feeling out of control or overwhelmed can be caused by sudden changes in the balance of estrogen, testosterone and progesterone or also from adrenal stress imbalances.
- Skin issues: Adult acne is associated with polycystic ovarian syndrome (PCOS), a hormonal condition that also causes irregular or absent menstrual periods due to ovulation irregularities.
- Hair loss/unusual hair growth: Imbalances in thyroid function or between estrogen and testosterone can cause thinning hair, and high levels of testosterone (such as in PCOS) can lead to unusual hair growth, including on the face.
- Infertility: Women with PCOS often have high amounts of androgens (including testosterone) as well as insulin resistance. Both contribute to increased estrogen, along with lack of ovulation and infertility.
- Fatigue/loss of energy: Fatigue can occur even when you get plenty of sleep, leaving you feeling physically and emotionally drained. Thyroid imbalances and chronic stress are the most likely contributors to this debilitating symptom.
You can stop hormonal imbalance from getting worse
At every age, your hormones are fluctuating on a daily basis, in mostly predictable patterns. But sometimes your hormones fluctuate more dramatically: puberty, pregnancy and perimenopause. When the changes become too extreme, or if your hormones can’t return to natural balance, you’ll experience problems.
To begin with you may sense that something is “off” or “not quite right” in your body. Then as the hormonal imbalance intensifies, you can experience physical and emotional symptoms that could become severe. Eventually, an imbalance worsens, symptoms can multiply, or their severity and frequency can increase.
The longer it goes on, the harder it can be to get back to a state of hormonal equilibrium; so it pays to take action sooner rather than later.
It’s good to listen to your symptoms
It can be a “eureka” moment when you first notice symptoms because they’re sending a clear message that your body is trying to juggle too many demands without getting enough support.
Even if PMS isn’t a problem and you’re not yet in menopause, you can still experience symptom-producing imbalances. Imbalances can occur in the ratios between estrogen, progesterone, testosterone and also with other hormones in your neuroendocrine system.
When your body doesn’t get the necessary basics every day on a consistent basis, it’s more likely that you’ll develop one or more of the conditions related to hormonal imbalance:
- Menstrual irregularities
- Polycystic ovarian syndrome (PCOS)
- Estrogen dominance
- Blood sugar imbalances, including insulin resistance
- Progesterone deficiency
- Androgen imbalance
For issues like these, many conventional practitioners focus only on estrogen levels. While estrogen is important, so are progesterone and testosterone — especially their ratios to each other. The levels of other hormones, like insulin, cortisol and thyroid, also matter. For example, estrogen levels may appear to be too high, but on closer examination, those can be holding steady while instead, it’s progesterone levels that are dropping.
Answer when your body asks for help
If you know you have hormonal imbalance symptoms, then you can provide the targeted support your body needs to naturally rebalance its hormones. Effective natural options can help resolve the root cause of all your symptoms, not just a select few.
You can take our Hormonal Imbalance Quiz to find out more about your symptoms, whether or not you are near menopause. Our Symptoms section is another helpful tool for exploring your hormonal health, including other signs of hormonal imbalance beyond the 7 listed above.
It’s also important to know that you can relieve your symptoms and feel better even if you’re frustrated right now.
Taking actions such as eating right and supplementing your nutrition, adding movement to your day and reducing the impact of daily stressors will tell your body that the hormonal emergency is over and that will make all the difference.
References and further reading
Mayo Clinic. Polycystic ovary syndrome (PCOS): Symptoms. Mayo Clinic Web site. Accessed May 1, 2016.
WebMD. Menopause and Perimenopause – Symptoms. Last updated February, 2014. WebMD Web site. https://www.webmd.com/menopause/tc/menopause-and-perimenopause-symptoms.Accessed May 1, 2016.
Badawy A, State O, Sherief S. Can thyroid dysfunction explicate severe menopausal symptoms? J Obstet Gynaecol. 2007 Jul;27(5):503-505.
Avis NE, Brockwell S, Randolph JF Jr, et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women’s Health Across the Nation. Menopause. 2009 May-Jun;16(3):442-452.
Weber MT, Maki PM, McDermott MP. Cognition and mood in perimenopause: a systematic review and meta-analysis. J Steroid Biochem Mol Biol. 2014 Jul;142:90-98.
Wathen PI, Henderson MC, Witz CA. Abnormal uterine bleeding. Med Clin North Am. 1995;79(2):329-344.
Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003 Jun;88(6):2404-2411.
Pedersen SB, Jønler M, Richelsen B. Characterization of regional and gender differences in glucocorticoid receptors and lipoprotein lipase activity in human adipose tissue. J Clin Endocrinol Metab. 1994 Jun;78(6):1354-1359.
Meier U, Gressner AM. Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin Chem. 2004 Sep;50(9):1511-1525.
Hudson T. Premenstrual Syndrome. In: Pizzorno JE, Murray MT, eds. Textbook of Natural Medicine. 4th ed. St. Louis, MO: Churchhill Livingstone; 2013: 1740.
Mayo Clinic. Polycystic ovary syndrome – Complications. September 3, 2014. Mayo Clinic Web site. Accessed May 1, 2016.
Randall M. The Physiology of Stress: Cortisol and the Hypothalamic-Pituitary-Adrenal Axis. February 3, 2011. Dartmouth Undergraduate Journal of Science Web site.
Christianson A, Murray MT. Hypothyroidism. In: Pizzorno JE, Murray MT, eds. Textbook of Natural Medicine. 4th ed. St. Louis, MO: Churchhill Livingstone; 2013: 1473.













