Authored by Dr. Mary James, ND
Urinary incontinence is extraordinarily common for women — but nobody wants to talk about it. I know, because I’ve experienced it.

In fact, nearly all women suffer at some point in their lives from some form of urinary incontinence. Bladder control issues can take us by surprise, changing from moderate (or nonexistent) to sometimes severe when menopause starts.
We should talk about urinary incontinence. Because otherwise, how are women going to find answers? Incontinence may not be entirely avoidable as we get older, but it is certainly treatable. And there are very effective alternative methods. Here’s what can be done both to prevent and to find relief from the common menopause symptom of bladder problems.
What is female urinary incontinence?
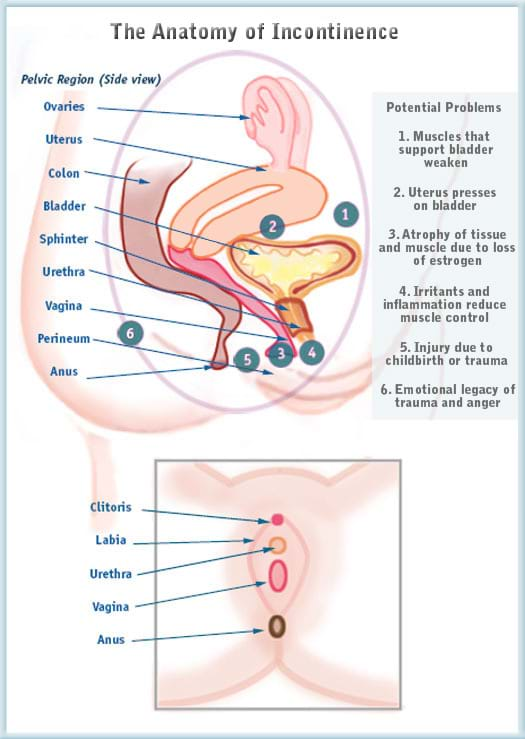
Involuntary leakage of urine, frequent urination, and a sudden urge to go to the bathroom, are all forms of urinary incontinence, which is generally defined as a lack of bladder control. While there are many causes, the most common cause is a gradual weakening of the pelvic floor muscles, nerves and tissue integrity that are meant to work together to control urination.
This is often caused by the stretching and atrophy of pelvic muscles due to age, pregnancy, gravity or trauma. Muscles can lose their elasticity as a result of pregnancies (especially more than one) or carrying extra weight. And tissue membranes and sphincters can become less efficient with a loss of estrogen at menopause. Organs such as the uterus are then able to move around too freely, often pressing on the bladder itself. In some cases, the bladder or urethra may become damaged or chronically inflamed, and malfunction. Scarring from surgery, injury or infection may disrupt the natural alignment of the organs inside the pelvic area.
How your bladder works
When your bladder is full, pelvic nerves send a signal to the brain that you need to urinate. Your pelvic muscles, especially the sphincter of the urethra, clench and hold until you get to the bathroom. Once you’re there, your brain tells the sphincter muscles to relax and your bladder empties.
To the right, you’ll see an illustration of factors that can lead to urinary incontinence. Here are just a few things to keep in mind:
- Your anatomy relies on the strength and tone of your pelvic muscles and ligaments, particularly the pelvic floor and perineum, to keep everything in its proper place.
- There is a lot of complexity in a small area — where your urinary tract, your reproductive tract and your intestinal tract all converge. Changes in one of these systems can easily affect one another.
- The bladder — and all the pelvic tissues and organs — are exposed to so many adverse developments, from posture to digestive problems. Some of these are unfortunately inevitable as we get older.
Types of bladder problems
Once you have a better idea of what type of urinary incontinence you’re experiencing, you’ll have a better chance at addressing the root causes. The most common types of bladder problems that lead to urinary incontinence include the following.
Stress incontinence
Stress urinary incontinence or light bladder leakage is related to the weakening of the pelvic floor. This results in pressure (or stress) on an otherwise fully functioning bladder.
I know very few women who have not experienced some degree of stress incontinence at some point or another. One minute you’re laughing, sneezing or coughing, and in the next moment you realize your underwear is wet. Exercise (particularly jumping), orgasm and even hearing running water can trigger it — often with greater regularity after menopause. While pregnancy and childbirth are frequently the cause of later stress incontinence, you can still suffer from stress incontinence if you’ve never had children.
Urge incontinence
Urge incontinence or overactive bladder (OAB) is a sudden, uncontrollable need to use the bathroom, even if you just went. It’s a result of uncontrolled contractions of the bladder muscle (the detrusor), caused by a disruption in communication between the bladder and the brain. This happens due to inflammation of the bladder lining, infection, injury, natural age-related atrophy or other reasons. Waking up once to several times at night needing to urinate, called nocturia, is common, as is accidental wetting due to an unstoppable urge to urinate. Sometimes overactive bladder is the result of overflow incontinence (see below).
Prescription medications for urge incontinence can either relax the detrusor muscle (e.g., Sanctura) or block the nerve impulses that prompt the bladder to contract (e.g., Detrol). They can be helpful for OAB, but they do not relieve symptoms of stress incontinence. They can also cause many side effects, including dry mouth, constipation, headache, blurred vision and dizziness, to name a few.
Many women experience a combination of both stress and urge incontinence, which is known as mixed incontinence.
Overflow incontinence
Overflow incontinence occurs when you can’t completely empty your bladder. This can happen when muscle tone is weak or you have a blockage. Symptoms of overflow incontinence include dribbling, urgency, hesitancy, straining, a weak urine stream or low urine production even though your bladder feels full. It’s more common in men, but overflow incontinence occurs in a significant number of women as well.
Less common causes urinary incontinence in women
A weakening of the pelvic floor muscles is the most common cause or urinary incontinence in women. But another possible cause is overstretching and herniation of the smooth muscle of the vaginal wall. This allows the bladder or urethra to balloon through the weakened muscle, creating a pocket in the vagina known as a cystocele or urethrocele. Because this makes it difficult to fully empty the bladder or can stretch the opening of the urethra, stress incontinence results.
You can usually feel a cystocele or urethrocele as a smallish, smooth bulge in the anterior (front) or side wall of your vagina. Overstraining, childbirth, and injury are the most common causes of cystoceles and urethroceles prior to menopause. After menopause, the natural thinning of the muscles is the more common culprit.
Chronic infection, surgery, medications (including synthetic HRT), radiation, adhesions, and disease are other factors that affect bladder function and the architecture of the muscles and nerves in the pelvis — and they can all contribute to incontinence.
You are more likely to develop urinary incontinence if:
- You have had a hysterectomy (see below).
- You are going through menopause (see below).
- You have had significant trauma to the pelvis, spine or bladder, surgery, or have a disability or impaired mobility (which can make it hard to get to the bathroom).
- You have suffered from a stroke, Alzheimer’s, multiple sclerosis (MS) or other central nervous system condition.
- You use medications that can cause a loss of bladder control.
- You smoke, are obese or have chronic constipation (with straining).
Systemic yeast, local yeast infections, and food allergies also play a role in bladder infections and interstitial cystitis, a painful bladder syndrome that typically features more urgency than incontinence. And, as in all inflammatory conditions, our emotions play a role in fueling the fire.
Incontinence and hysterectomy
Hysterectomy increases the odds of incontinence for two main reasons: the design and support of the pelvis is permanently changed as a result, and women often lose the muscle-toning effects of their natural sex hormones post-hysterectomy, even if their ovaries have not been removed.
A radical hysterectomy can cause extensive scarring that disrupts your inner musculature and nerves. Many surgeons are now capable of performing a laparoscopic hysterectomy, which involves far less damage, or a modified procedure to ablate the uterine lining or embolize the arteries to the uterus without doing a hysterectomy.
Keeping your ovaries is important when it comes to incontinence because of the beneficial effects of estrogen on the muscles of the bladder, bladder lining, and urethra and on the connective tissues within the pelvis. Even so, in over half of women receiving hysterectomy, those who keep their ovaries still suffer some loss of ovarian function after the procedure.
Studies also show that synthetic hormone replacement therapy increases a woman’s risk for stress incontinence — just one reason that we don’t recommend synthetic HRT in any form. Topical bioidentical estrogen clearly helps promote a natural elasticity and suppleness in the pelvic floor. Women with urinary incontinence may respond extremely well to bioidentical estrogen cream applied directly to the vaginal wall and particularly the area near the urethra.
Bladder control and menopause
The relationship between bladder control and hormonal balance becomes increasingly important as we get older and transition through menopause. During menopause, a decrease in estrogen initiates a thinning and weakening of the pelvic muscles and connective tissue.
I’m seeing more ads for pharmaceuticals directed at female incontinence. But, as usual, they only address the most obvious symptoms and do nothing to treat the underlying loss of muscle tone. Most of the drugs available act on the muscle spasms related to overactive bladder, but do not treat stress incontinence. What’s more, they can cause bothersome side effects.
As with any drug or hormone, you need to weigh the long-term risks against the potential benefits before taking a pill that might do serious long-term damage to your health. Of course, we recommend you try the most natural steps first, and resort to drugs only if necessary to get symptom relief.
After menopause, women are more prone to urinary tract infections (UTI), especially bladder infection, or cystitis. As the urethral muscle loses strength and elasticity due to loss of estrogen, pockets of bacteria can flourish. Taking an antibiotic — nowadays it’s typically a one-day massive dose — is usually enough, but in some cases inflammation takes hold and damages the lining of the bladder.
This multi-factorial condition, called interstitial cystitis (IC), is a growing concern in women’s health. It’s an inflammatory condition that has all the symptoms of a urinary tract infection even when no bacteria are present. Although there are many triggers and proposed causes of IC, it would not surprise me if estrogen imbalance is sometime implicated in the escalating rates of interstitial cystitis that I’m seeing.
Urinary incontinence treatment — what you can do right now
Bladder issues are like so many other health-related concerns — the sooner you attend to them the easier they are to treat. You may want to try the following for incontinence.
Talk with your healthcare provider
If you are noticing any urine leakage or an increased frequency of urination, the first step is to get checked out by your healthcare practitioner. Depending upon the situation, you may find it useful to consult further with a gynecologist, urogynecologist or urologist. Most women suffer from some form of mixed incontinence that usually can be treated with alternative therapies.
Pelvic floor exercises
Incontinence can often be arrested or reversed with simple Kegel exercises alone. You can do them anywhere, anytime — and you should.
To do a Kegel, imagine that you are trying to stop yourself from urinating. Practice both short and long Kegels. You can even do an anticipatory Kegel before you sneeze or cough and prevent leakage!
A wonderful added benefit of Kegels is that the increased muscle tone can increase sexual pleasure in both sensation and orgasm.
Sometimes women have trouble identifying the muscles that control the bladder, so get frustrated attempting Kegels. This can be a natural result of conditioning the brain to ignore bladder stimulation. How many of us are too busy to go to the bathroom when we feel the urge, and then “forget” we had to go? Over time, it’s possible that our brain just stops paying attention and we disconnect. It can take some work to get those pathways talking again.
If Kegel exercises don’t seem to be working well for you, you can try insertable cones or balls (available through your doctor or on the internet) to help train your PC (pubococcygeal) muscle. Biofeedback practitioners use electronic monitors inside the vagina to help women learn how to identify and tone muscles related to the bladder. Both tools can be very effective.
Any kind of physical exercise that engages your core will help strengthen your pelvic muscles, but Pilates and yoga, in particular, are great inner toners. Both focus on building a firm core or root. They also use deep breathing and mindful movement to reconnect the brain to the body.
Acupuncture
Acupuncture is another method that has provided symptom relief for some women. It helps tone muscle and increase blood flow to the bladder. It can boost the immune system, soothe inflammation, and restore balance to the hormones.
Pelvic physical therapy
Pelvic physical therapy (PPT) is sometimes effective in difficult cases. Practitioners use several diagnostic tools, including sonograms, physical exams and lower back screenings to evaluate the cause of incontinence. Treatment may include external and internal pelvic floor massage, relaxation training, biofeedback, strengthening, bladder retraining and home exercises. This is especially useful when patients have adhesions or physical anomalies due to radiation treatment, injury or surgery. Many women who undergo PPT report increased libido and enjoyment of sex in addition to better bladder control.
Nutrition
Nutrition is vital to restoring a healthy balance to your endocrine and immune system, which in turn is important for maintaining muscle tone and preventing infection. Eating a diet of whole foods with plenty of fruits, vegetables, protein and some whole grains will help level out your hormones. Take a multivitamin, multi-mineral formula to support your body.
Allergies may exacerbate an overactive bladder. If you think you may have food allergies or sensitivities, we recommend trying an elimination diet (avoiding all suspect foods for two weeks, then re-introducing one at a time for two days).
Stay hydrated
Drink plenty of water and herbal tea. Flushing your urinary tract regularly will help evacuate bacteria. Cranberry — in the form of juice, supplement or extract — can help prevent urinary tract infections by changing the pH of the bladder and preventing bacteria from attaching to the bladder wall, but choose one with no added sugars. (Excess simple carbohydrates in the diet only encourage UTIs.) If you are getting up in the middle of the night to urinate, stop drinking liquids a few hours before bed.
Internal or surgical methods
If urinary incontinence is keeping you from fully enjoying your work, love life, hobbies and pursuits, then fitted internal devices or surgical interventions are a reasonable next step. Some women find this necessary after a few pregnancies.
Fitted pessaries, sometimes referred to as prolapse pessaries, are removable umbrella-like support rings that can help lift your pelvic organs up off your bladder. A pessary can be a great non-invasive choice for a woman with a cystocele or uterine prolapse.
Bladder laparoscopy and bladder slings can be helpful for treating severe stress incontinence in some women. Currently the most common procedures are known as the Burch colposuspension technique and the fascial sling. In the past, bladder suspension surgeries had a useful life of about four years. In the Burch, the urethra and bladder are secured with sutures to the pelvic wall. The new bladder slings use life-like materials that move with the body and act like real muscle.
As with any surgery, we recommend getting as much information as possible and discussing your options with a few practitioners. There are now gynecologists who specialize in urology (urogynecologists), and more women are going into urological surgery (formerly an exclusively male specialty). It’s safe to say that the more experience a surgeon has with a procedure, the more likely it is that you will experience the results you are looking for.
You don’t have to live with incontinence
I know there isn’t an easy remedy for urinary incontinence. But as with so many problems with our bodies, let’s focus on what we can control — because that’s how we’ll find solutions for menopause and reduce early menopause symptoms. I feel for every woman whose life is compromised by urinary incontinence! With a willingness to talk about it and experiment with changes, you can feel a great improvement.