Authored by Dr. Susan E. Brown, PhD
The National Osteoporosis Foundation recommends that all women over 65 years old, as well as all postmenopausal women with at least one risk factor for osteoporosis have their bone mineral density (BMD) tested. Why are we waiting this long? In our opinion, all women should be carefully screened for risk of fracture at a much earlier age — no later than age 40! Then, if their fracture risk assessment reveals concern, women at risk would undergo bone density testing right away (if we could convince insurance companies to pay for it). This would allow us to see when women need to take steps to improve bone health. And it would give us a baseline to compare future tests against. Then we could track how well their bone building programs are working.
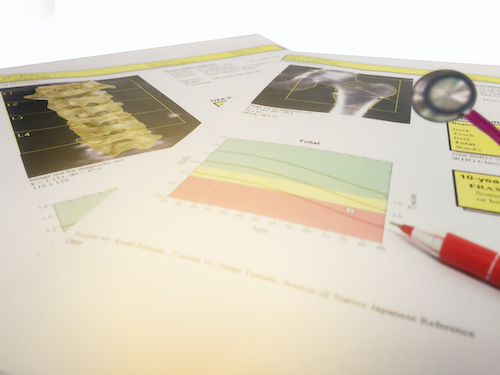
What is a DEXA scan?
Today, the most common way to look at bone mineral density is with a DEXA scan (often referred to as DXA). But rather than actually measuring the density, this technology focuses low-energy x-rays from two different sources onto the bone and measures the proportion of light rays that pass through the tissue. These data are fed to a computer that plugs them into a formula to calculate an average of the bone mineral content of any part of the skeleton, typically the spine, hip, wrist and femur. The theory is that the more light that passes through, the less mineral mass present in the bone.
This test can be helpful in determining how “dense” bones are, but not necessarily how strong they are. Nor do the test results tell us when we lost density. It could have occurred in the remote past, or just last month. Our bones naturally get thinner as we age, but keep in mind: thin doesn’t necessarily mean you’ll fracture. Bone strength actually comes from its microarchitecture, which is partly a function of genetics. It also comes from its ability to self-repair, which is largely a function of a woman’s life history and whole-body wellness. In other words, a woman may have thin bones on DEXA, but have great architecture and capacity for self-repair. And never have a fracture in her life.
How is a diagnosis made?
This is another one of the problems with our current testing model. First, we give a woman a number called a T-score. This is based on how she compares to the average bone mineral density of a group of women between the ages of 20 and 29. If our bones naturally get thinner as we age, of course a woman at 60 is going to have a different T-score than a woman in her 20’s! Next, conventional medicine gives a woman a diagnosis of osteoporosis if she is 2.5 standard deviations away from this standard. Osteopenia is diagnosed if she deviates between 1.0 and 2.4 from the standard.
The more helpful and accurate measurement is the Z-score. This compares your numbers against the average BMD for your age, sex, weight, and ethnic or racial origin. But focusing on the T-score is the gold standard for today’s practice. This is a shame because many women are diagnosed with osteoporosis and osteopenia, and believe they need to immediately go on Fosamax or some other powerful drug to preserve their bones. In reality, this may be unnecessary.
The truth is we can maintain strong and healthy bones throughout life with quality nutrition and plenty of exercise. So scrutinize all your fracture risk factors. If possible get tested while still in early perimenopause. You can then use your score as a reference point for interpreting future test results. And place your DEXA results in the context of other women your age. If you’re interested in tracking your bone health and cannot justify the expense for DEXA, you might consider NTx testing.
See our articles on osteoporosis and bone health for more information.









